Articles and most recent
Navigating Your First Dental Practice Purchase: Red Flags to Watch For
As a young dentist on the cusp of buying your first dental practice, the Read more>
Dental Practice Due Diligence: What the Buyer Should Know About the Accounts Receivable and Patient Credits
Due diligence is one of the most important jobs for dentists buying a practice Read more>
Five Trends that will Impact Dental Practice Transitions in 2024
As we step into 2024, five trends are emerging that may impact dental transitions Read more>
Don’t Leave Money on the Table: Benefits of Owning a Dental Practice vs Working for Someone Else
There are many compelling benefits of owning a dental practice and ensuring maximum earning Read more>
Understanding Insurance Credentialing in Dental Practice Transitions
The Role of Insurance Credentialing in Dental Practice Transitions Insurance credentialing is a ‘necessary Read more>
13 Reasons Why You Should Be Practicing Rural Dentistry
Big City Lights vs Small City Bites: Why You Should Consider Practicing Rural Dentistry Read more>
Preparing for Your Dental Practice Sale in 5 Years
Retiring and selling your dental practice is one of the most significant events in Read more>
Dental Student Loan Repayment Strategies for 2023-2024
After a delightful 3-year break from payments, as well as interest accrual on student Read more>
Avoid the “Potential” Pitfall When You Sell Your Dental Practice
Selling a dental practice can be challenging and ensuring that you sell your dental Read more>
Creating an Employee Handbook for Dental Practices
Most dental offices are not large enough to have a full-time human resources employee. Read more>
Should You Sell the Accounts Receivable in a Dental Practice Transition?
Should You Sell Your Accounts Receivable? The short answer to this question is yes, Read more>
Five Things Every Dentist Should Know About Disability Insurance
The odds of a dentist experiencing disability is a lot higher than most people Read more>
What is EBITDA?
EBITDA – six letters that can make all the difference in your dental practice Read more>
Understanding Dental Practice Purchase Agreements
Basic Understanding of Key Dental Practice Purchase Agreement Elements Understanding key elements in a Read more>
Is Your Life What You Thought it Would Be as a Dentist?
Remember that first time you didn’t have all summer for vacation? Summers off were Read more>
Women in Dentistry: Why Owning a Practice is the Right Path
I have been a dental practice broker over 20 years now after owning a Read more>
Tactful Tips for Announcing a Dental Practice Transition
Tips for Announcing a Dental Practice Transition Transitioning your dental practice requires balancing the Read more>
Dental School Debt Repayment Strategies for a Smart Future
Dental School Debt Repayment: Smart Strategies for Your Future It’s common for an engagement Read more>
What Can a Buyer do to Ease Negotiations with a Seller?
Make a Good Impression It may sound like common sense, but the best thing Read more>
Navigating the Contracts and Negotiations for a Dental Transition
Contracts, and the negotiations that surround them, are a significant part of the dental Read more>
Should You Build or Buy a Dental Practice?
In today’s economic climate, dentists are becoming increasingly discouraged by the shortage of available Read more>
The Roadmap to a Successful Life After Practice
I agree with Madeleine Albright, former Secretary of State, when she said, “Every step Read more>
Need to Catch up on Your Dental Retirement Savings? Here’s One Way.
Dentists are increasingly getting a late start on saving for retirement. This is often Read more>
What You Need to Know About Private Practice vs. DSO
DSOs are here to stay. They are spreading nationally, and many believe they will Read more>
Is Your Staff Making the Most out of Social Media?
Did you know 63 percent of social media users under the age of 35 Read more>
When Selling a Dental Practice, Make Sure You’re Following Expert Advice
Recently, a retiring doctor perused the website of a large and trusted dental insurance Read more>
Determining the Listing Price of a Dental Practice
The single-most important factor in determining the practice sales price is the collection total Read more>
The Upside of Merging with Another Dental Practice.
Mergers are unquestionably the best return on investment you can make. The success of Read more>
Dental Practice for Sale by Owner
Planning Dental Practice for Sale by Owner Can be Daunting. Take our Quiz to Read more>
Buying a Dental Practice? Here Are Some Important Questions to Get Answered.
Buying a Dental Practice? Consider Asking These Questions First. If you’ve decided to buy Read more>
An Exclusive Sale Listing – Why Would I Do That?
You’re ready to sell your practice and you want the best result possible, so Read more>
Six Questions Every Dentist Should Ask if You’re Thinking of Selling to a DSO
Be Sure to Ask These Six Questions When Considering Selling to a DSO In Read more>
If something happened to you, who would know the value of your practice?
Do you know the value of your dental practice if something were to happen Read more>
Due Diligence: What does it mean?
Due diligence is a phrase becoming more commonly used by buyers in the market. Read more>
Understanding How Dental Practices are Valued
There are many reasons why dentists might want to have their practices appraised. Some Read more>
Should you sell your dental practice to a DSO?
What is a DSO? A DSO (dental service organization) contract with dental practices and Read more>
Hope for the Best, Prepare for the Worst
None of us want to discuss or think about death or long-term disability. Humans Read more>
10 Reasons Why You Should Use a Dental Broker
Many of us have probably heard from individuals who think sellers don't need a Read more>
Should I Stay or Should I Go?
Life is like a record album for those who remember what that actually is. Read more>
An After-Hour Training Opportunity
Using your practice as a Dental Assisting School The U.S. Bureau of Labor projects Read more>
The Win-Win Practice Transition
The classic definition of a dental practice transition is when a doctor sells all Read more>
The Smart Money is Buying Dental Practices Now!
Investing in a Dental Practice is a Smart Investing Move The United States had Read more>
Dental Practice Financing in a Post-COVID Economy
Whether you are a first-time dental practice owner or someone looking to expand, relocate Read more>
The Cost of Dental Practice Valuation
A dental practice valuation is much like a preventative checkup on your practice’s financial Read more>
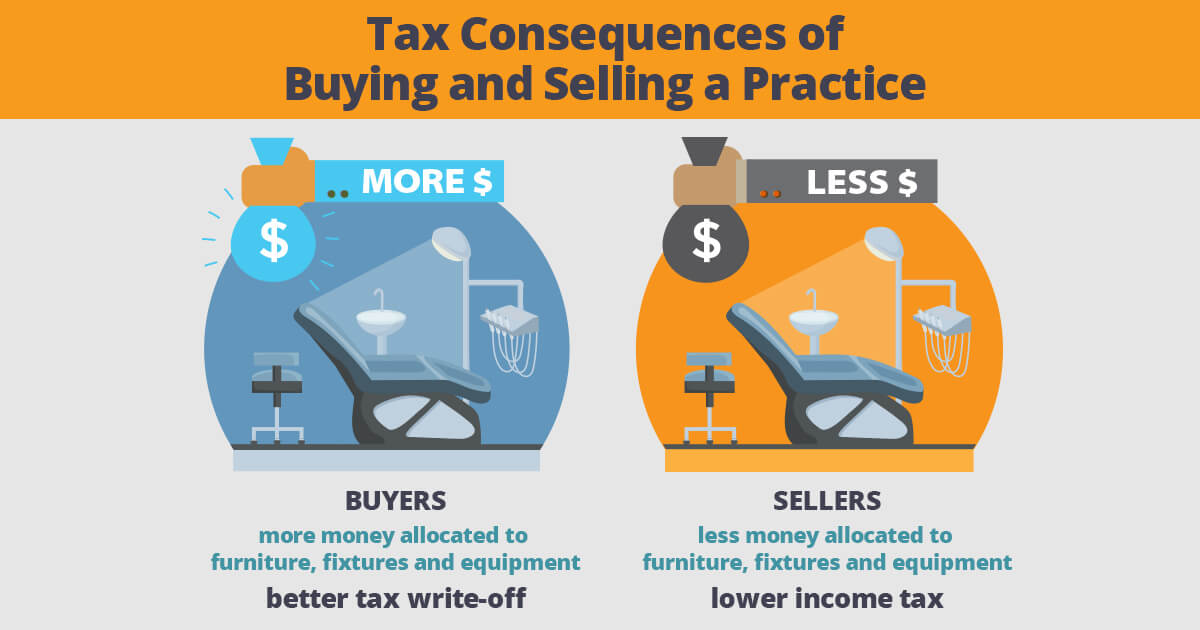
Tax Consequences of Buying and Selling a Practice
Consider the Tax Consequences When Buying and Selling a Dental Practice Calculating dental practice Read more>
Your Multimillion-Dollar Decision
If you’re a dental student or new graduate, you’re going to be faced with Read more>
Avoiding Practice Transition Problems
I would like to share some stories with you concerning a few of the Read more>
Buy a Practice…Now???
COVID-19 has all of us questioning how we move forward. Unfortunately, many will retreat Read more>
Financing for Dental Practices Today
Whether you are a first time practice owner or someone looking to expand, relocate Read more>
10 Tips To Prepare for a Dental Practice Sale
Use Downtime as an Opportunity to Add Value to Your Dental Practice Sale We Read more>
The Advantages and Disadvantages of Selling to a DSO: A Case Study
What are DSOs? DSOs actually go by a number of different names: Dental Service Read more>
Millennial Dentists & Changes in Dentistry
“MILLENNIALS” are people born between 1980 and 2005.1(p3) They’ve grown up in a much Read more>
What Do You Do After Dental School?
Things to Consider After Dental School? After graduating from dental school, you’ll need to Read more>
What are Some of the Best Ways to Sell a Dental Practice?
If you are healthy and just want more free time, you are fortunate to Read more>
How to Start a Successful Dental Practice
WHAT THEY DIDN’T TEACH YOU IN DENTAL SCHOOL Most of us graduated from Dental Read more>
How to Buy a Dental Practice
After completing your formal training and saving money for a down payment, you might Read more>
Things to Look for in Your Associate Dentist Employment Agreement
If you get a job as an associate dentist you are typically confronted with Read more>
Understanding EBITDA (Earnings Before Interest, Taxes, Depreciation, and Amortization)
An understanding of the value of a dental practice is essential not just for Read more>
Case Study: Transfer of Accounts Receivable, with a Wrinkle
A recent practice transition that we handled included the purchase of the selling Doctor’s Read more>
The $14,000,000 Decision Every Dentist Must Make
Suppose that when you begin your dental career that you will have to check Read more>
The Dental Practice Transition Period
There are many issues that have to be agreed upon in order to sell Read more>
The Associate Buyout
by Bill Avery, DDS, PhD As happens with most dental practice brokers, I frequently get Read more>
How to Increase the Profits of Your Dental Practice Sale
There are many factors to be considered when attempting to increase the value of your Read more>
11 Steps to Evaluating a Dental Practice
Evaluating a dental practice for sale is a multi-step process. If steps are skipped, problems Read more>
Merging a Dental Practice Basics
Nowadays you can almost assume that most dentists will have to go through the Read more>
Sell Your Practice Now and Stay on After the Sale
What if you could sell your practice and office space at the FAIR MARKET Read more>
Perils for Practice Transition: Double Taxation of Goodwill
For most dental practices, goodwill constitutes the largest component of the practice’s value. A Read more>
The Best Reasons to Own
Today, if you are a dentist and do not own all or part of Read more>